A rabid raccoon attack on Durham resident, Christine Houghton, earlier in May this year has raised concerns about rabies awareness across the country. So, what does the path to improving public notification of rabies cases look like? Before we get into it, here’s a bit of background on rabies.
What is rabies?
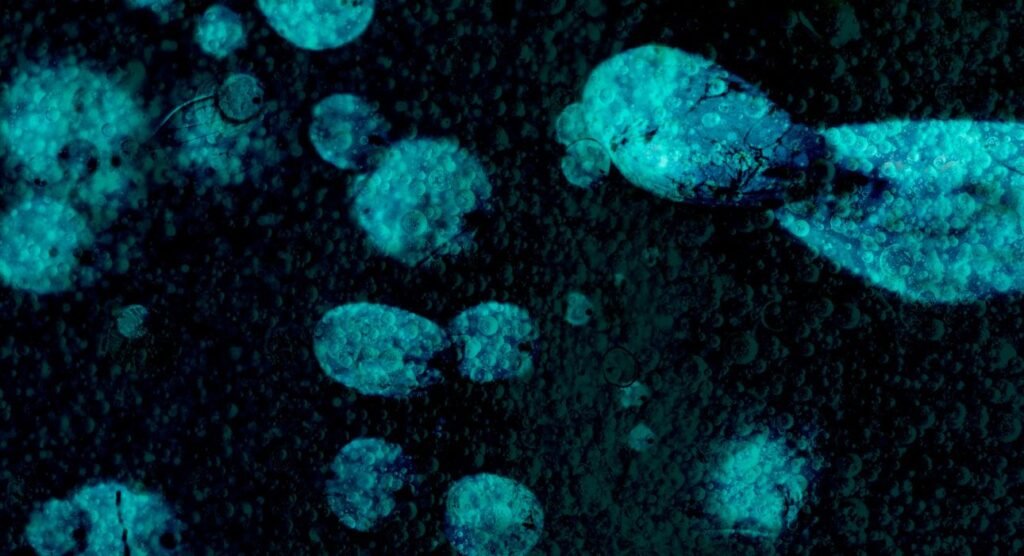
Rabies is a rare virus, estimated to kill fewer than 10 people a year in the United States, but it’s still a serious public health concern for the country. It’s near-fatal for anyone infected and can greatly impact wildlife. This viral disease can cause encephalitis in humans and other mammals, like dogs, bats, and most famously in recent times—raccoons. Once clinical symptoms start to appear, the disease is virtually 100% fatal.
Rabies causes encephalitis, which is the inflammation of the brain. Encephalitis is most commonly associated with flu-like symptoms, like headaches, fevers, aches, and fatigue or weakness. The rabies virus also affects the central nervous system, leading to a range of symptoms, including psychiatric and neurological manifestations. For those studying online psychiatric nurse practitioner programs or similar, the effects of rabies are a common topic.
Rabies is transmitted through the saliva of infected animals. It typically spreads by the infected biting another animal or person. In rare cases, the disease can also spread when infected saliva gets into an open wound or the mucous membranes. It’s estimated that 70,000 people around the world die of rabies every year. While rabies prevention, through animal control programs and human/animal vaccinations over the past century, the disease is still a massive public health issue.
The history of rabies
Rabies is one of the oldest known diseases with cases dating back to 4000 years ago. Interestingly enough, for most of human history—a bite from a rabid animal was seen as a death sentence. Historically, rabies was previously known as ‘hydrophobia’, as it would induce panic in the infected individual when presented with liquid to drink.
Almost all human exposure to rabies through saliva or a bite was fatal until a vaccine was developed in 1885, by Louis Pasteur and Emile Roux. Now immunizations for rabies before exposure are common, used for both human and nonhuman populations. Many regions in the United States require domesticated animals to be vaccinated against rabies. This includes vaccinating dogs, cats, and ferrets.
What are the risks of rabies?
Beyond being an extremely serious and fatal disease among humans, rabies can also be a major risk to pets, like cats or dogs. Animals that are infected with the virus, unfortunately, suffer a painful death. They also have a personality shift, resulting in abnormal and aggressive behaviour, which also increases the risk of transmission. Rabies also poses an extreme psychological and social impact. The threat of the virus can cause significant fear and panic in communities during an outbreak. It can also cause trauma to those exposed to the virus, particularly children. The virus can also pose significant challenges to wildlife conservation. It can threaten endangered species if the virus outbreaks in the population, disrupting ecosystems and conservation efforts.
What are the current protocols regarding rabies?
The United States has protocols regarding reporting and managing rabies for wildlife, as well as treatment in the case of potential transmission. It’s recommended that civilians don’t interact with or handle wild animals, and report any cases of potential rabies sightings. The National Rabies Management Program also exists for managing the spread of wildlife rabies. The program was established with the goal of eliminating terrestrial rabies in the United States. This program is employed by Wildlife Services in conjunction with local, State, and Federal governments, universities, and other organizations by distributing oral rabies vaccinations in areas to target wild animals.

How does treatment work?
Once a rabies infection is established, there’s no effective treatment for it. Though a small number of people have survived the disease, with only fourteen documented cases as of 2016, infection typically leads to death. If you’ve been bitten by an animal that is suspected to have rabies, it’s possible to receive a series of shots to prevent the virus from infecting you.
If you haven’t had rabies vaccinations previously, you’ll receive four injections over 14 days. If you have been previously vaccinated, you’ll get two injections over three days. Fortunately, most states require rabies vaccinations as a preventative cause for most domesticated animals. The vaccine is also highly recommended for humans to decrease the risk if bitten and is sometimes required when travelling.
How can we improve communication with the public?
Timely and effective communication with the public regarding health concerns, like the rabies virus, is crucial for the protection of public health, preventing the spread of the virus, and reducing the risk of panic and misinformation. If communities are made aware of rabies outbreaks in local wildlife, it helps with informing the public to avoid the area and lowers the risk of potential transmission. Clear communication on the risks of rabies and how it spreads also encourages people to avoid risky situations and report potential exposure they see in local wildlife.
Misinformation regarding rabies and outbreaks can also cause unnecessary distress and panic in communities. Clear communication through public health channels, it’s a good way to get ahead of misinformation and ensure the public has accurate and updated information. Clear and timely communication also helps when it comes to coordinating emergency efforts between public health services, veterinary services, authorities, and the community. It allows all parties to stay up-to-date with the latest information and act accordingly.
Conclusion
Even though it’s rare, it’s evident that clear communication when it comes to a near-fatal virus like rabies is the most important thing on the path to improving public notification. We need to make sure the general public is kept informed on time while misinformation is eliminated to strengthen and protect public health.













Leave feedback about this